Topic of the Month: Rotator Cuff Injuries
Upper Crossed Syndrome is an umbrella term to describe a group of related postural dysfunctions. There are several commonalities in persons who have this condition.
About:
This month’s area of focus is one of the more commonly injured areas of the body, the shoulder, more specifically, the rotator cuff. The rotator cuff consists of four distinct muscles that control specific motions for the upper arm. These muscles include the supraspinatus, infraspinatus, subscapularis and teres minor. The supraspinatus muscle is situated along the top of the scapula (shoulder blade) and assists with elevation of the arm when raising it out to the side (abduction). Both the infraspinatus and teres minor function as external rotators of the shoulder, whereas the subscapularis is the major internal rotator of the shoulder joint. With rotator cuff injuries, one or more of these muscles/tendons could be fully or partially torn leading to pain and/or loss of function within the shoulder itself. Identifying painful or difficult motion in a specific direction can help lead to a working diagnosis and a baseline of where treatment can begin. If a suspected rotator cuff injury occurs and initial testing reveals weakness, pain or loss of function, further testing may be required to determine the extent of the injury. X-ray will show the integrity of the bony structures (humerus, clavicle, and scapula) to rule out possible fracture or arthritic changes. In order to determine if one or more of the muscles/tendons is compromised, an MRI could be ordered. This will show the degree of injury and whether there is a partial or full thickness tear to the region.
Population Affected:
Rotator cuff injuries are commonly seen with increasing age. It is estimated that 30% of persons aged 60 or older and 62% of persons over the age of 80 have a rotator cuff tear. (Source). Age related degeneration such as arthritis within the shoulder has shown to increase likelihood of rotator cuff injuries. Other factors such as aberrant posture, such as upper cross syndrome, can also predispose an individual to an increase in chance of a rotator cuff injury. There are genetically linked studies that show individuals who have rotator cuff-like injuries tend to be more at risk as well. However, rotator cuff injuries are not just for an aging population. Persons who suffer a traumatic injury such as a direct fall on the shoulder or pain following a throwing motion are at risk as well. Traumatic injuries are thought to be the primary cause of rotator cuff injuries in younger populations such as athletes. Repetitive motions such as throwing a baseball, hitting a tennis ball and volleyball are common ways to suffer a rotator cuff injury.
Effects of Rotator Cuff Injuries and Other Possible Diagnoses:
It is important to first confirm that the rotator cuff is the region of injury. Referred pain from the neck and brachial plexus can mimic shoulder injuries. This can be done by an orthopedic examination of the cervical spine and the shoulder that is potentially compromised. Once it is deemed that the rotator cuff is causing the issue, the most common finding is pain in the shoulder with associated weakness. This pain is often increased when laying on the shoulder or at night as well as with overhead activities. If surgical treatment is deemed to be unnecessary, it is important to keep the shoulder strong and mobile. Letting rotator cuff injuries heal by way of not using the affected limb could lead to complications such as a frozen shoulder (adhesive capsulitis). With frozen shoulders, range of motion in the shoulder is severely reduced and makes moving the shoulder in normal ranges of motion increasingly difficult over time. Also commonly mistaken for rotator cuff injuries is tendonitis to the shoulder muscles that comprise the rotator cuff. These can present with pain in the shoulder with specific motion oftentimes occurring from overuse of one or more of the muscles. Arthritis, bursitis, and labral tears are other common differential diagnoses for shoulder pain that can limit range of motion. As you can see, several shoulder injuries share a few common presenting symptoms, pain and loss of range of motion.
How Chiropractic and Massage Therapy Can Help:
It is important to note that full thickness rotator cuff tears could warrant surgical repair. With acute injuries to the rotator cuff, surgery could be recommended by the diagnosing doctor as well. Conservative treatment is often recommended before surgical intervention.
Chiropractic is a conservative treatment that can help address movement dysfunction with the shoulder as it relates to the scapula and the clavicle. Restoring proper movement allows the shoulder the best possible healing outcomes in terms of healing times and regaining function. Here at Lakeland Chiropractic, we can address those movement dysfunctions in the shoulder as well as the surrounding musculature. We often see nerve entrapment within muscles near or a part of the rotator cuff. Through cupping, dermal traction, and nerve flossing, we have seen patients’ make great strides in both increased function and decreased pain to the shoulder.
Massage therapy is a great conservative approach to help increase range of motion in the shoulder. Oftentimes with rotator cuff injuries or shoulder injuries in general, the surrounding muscles will become overactive to try and protect the injured joint. This in turn can lead to increased pain with motion of the shoulder even after the injury has healed. Therapeutic massage to the muscles will help increase the range of motion and release active trigger points that may have developed during the time where the shoulder was immobilized.
Combining both chiropractic care and massage therapy can help reduce pain and restore proper function to the shoulder.
References:
David Cruz, D. C. (n.d.). Preventing rotator cuff injuries with corrective exercise (part 1). NASM. Retrieved April 21, 2023, from https://blog.nasm.org/uncategorized/how-to-prevent-rotator-cuff-injuries-through-corrective-exercise-programming-part-1?cq_cmp=19767936423&network=x&utm_term=&utm_campaign=CPT_ACQ_SHOPPING_WEB_PMAX&utm_source=google&utm_medium=paidsearch&hsa_acc=2454829191&hsa_cam=19767936423&hsa_grp=&hsa_ad=&hsa_src=x&hsa_tgt=&hsa_kw=&hsa_mt=&hsa_net=adwords&hsa_ver=3&gclid=CjwKCAjwoIqhBhAGEiwArXT7K-xuNpoMKMIGOKMqFiDx48pa5_dJOcwfbZ99_XJPdhxOp2CjDhLMaxoCB8QQAvD_BwE
Dev, D. (2022, November 22). Rotator cuff tear symptoms. OPA Ortho. Retrieved April 21, 2023, from https://www.opaortho.com/rotator-cuff-tear-symptoms/
Disorders of the rotator cuff. OrthoPaedia. (n.d.). Retrieved April 21, 2023, from https://orthopaedia.com/page/Disorders-of-the-Rotator-Cuff
Gpaadmin. (2021, June 23). Rotator cuff muscle and rotator cuff injury: Bosic: Shoulder pain. Barangaroo Orthopaedic and Sports Injury Clinic. Retrieved April 21, 2023, from https://bosic.com.au/rotator-cuff-muscle/
Jonathan Cluett, M. D. (2020, December 5). What happens when you have a torn rotator cuff? Verywell Health. Retrieved April 21, 2023, from https://www.verywellhealth.com/rotator-cuff-tears-2549783
May T, Garmel GM. Rotator Cuff Injury. [Updated 2022 Jun 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK547664/
Rose, Michael & Noonan, Thomas. (2018). Glenohumeral internal rotation deficit in throwing athletes: current perspectives. Open Access Journal of Sports Medicine. Volume 9. 69-78. 10.2147/OAJSM.S138975.
Rotator Cuff. Physiopedia. (n.d.). Retrieved April 21, 2023, from https://www.physio-pedia.com/Rotator_Cuff
Rotator cuff strain - symptoms, causes, treatment and rehabilitation. Sportsinjuryclinic.net. (2023, February 22). Retrieved April 21, 2023, from https://www.sportsinjuryclinic.net/sport-injuries/shoulder-pain/acute-shoulder-injuries/rotator-cuff-strain
Rotator cuff tears - orthoinfo - aaos. OrthoInfo. (n.d.). Retrieved April 21, 2023, from https://orthoinfo.aaos.org/en/diseases--conditions/rotator-cuff-tears/#:~:text=In%20most%20rotator%20cuff%20tears,with%20lifting%20a%20heavy%20object.
StatPearls. (2023, March 27). Anatomy, rotator cufieved April 21, 2023, from f. StatPearls. Retrhttps://www.statpearls.com/ArticleLibrary/viewarticle/28651
Topic of the Month: Lower Crossed Syndrome
Upper Crossed Syndrome is an umbrella term to describe a group of related postural dysfunctions. There are several commonalities in persons who have this condition.
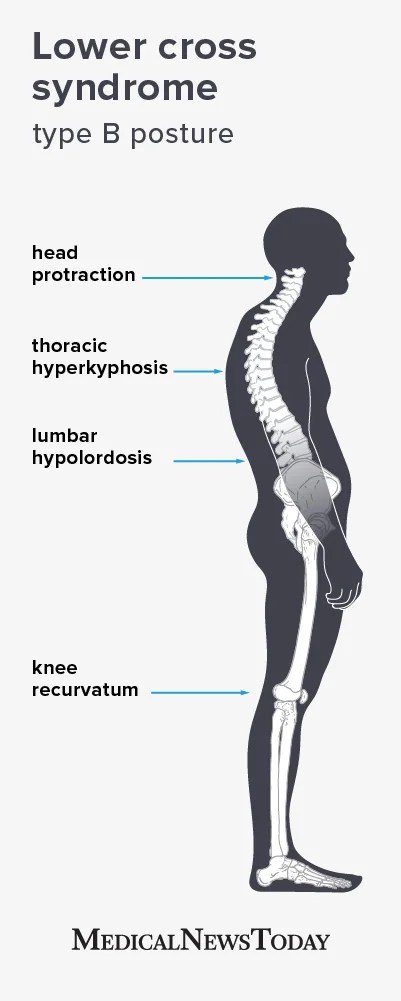
Welcome back to the topic of the month. The condition we have selected to highlight in this edition is Lower Crossed Syndrome. If you read last month's newsletter, you might recognize similarities in this month's topic. Lower crossed syndrome, like upper crossed syndrome, is a postural disorder in the lower thorax and pelvis characterized in two general presentations. In both presentations, muscle imbalance is prevalent; which is depicted in the images below.
Just like in upper crossed syndrome, lower crossed syndrome presents with a series of hypertonic (tight) and inhibited (weak) muscles that work in opposition to one another. Hypertonic muscles include muscles that comprise the hip flexors such as the psoas, rectus femoris, iliacus, sartorius and pectineus. On the posterior side of the body, hypertonic muscles in the low back such as the erector spinae and latissimus dorsi tend to be overly tight. Weak/inhibited muscles in lower crossed syndrome are located above and below the hypertonic muscles on their respective sides of the body. Inhibited core muscles such as the transverse abdominis, internal and external oblique can commonly be seen in lower crossed syndrome. Located below the erector muscles of the spine, are the glute muscles. With a lower crossed presentation, muscles such as the gluteus maximus, medius and minimus can become weak/inactive along with the piriformis which can lead to the overactivation of the muscles listed above that are commonly tight.
Population Affected:
Lower cross syndrome is typically most prevalent in persons who sit for extended periods of time. By frequently sitting for long periods of time, the muscles that create the lower crossed condition subsequently become overactive (tight) or inhibited (weak). Lower cross is commonly seen in elderly/aging individuals due to an increased amount of time being stationary or sitting around the house. People who sit at a desk during working hours are also prone to lower cross syndrome. At Lakeland Chiropractic we are beginning to see kids/adolescents who more frequently present with the signs/symptoms of lower crossed syndrome. Perhaps this can be traced back to sitting long hours in the classroom or at home when school is over. Lower crossed syndrome does not exclusively mean one sits too much or is underactive throughout the day; well conditioned athletes can present with signs of lower crossed as well. Repeated use and/or overuse of muscle groups can increase the chances of developing this postural condition. Minor injuries to one or multiple muscles associated with lower cross can in turn cause a chain reaction of sorts and manifest in the presentation of lower cross syndrome over time.
Effects of Lower Crossed Syndrome:
Perhaps the most common effect of lower crossed syndrome is the manifestation of low back pain. Due to muscle imbalance and the neurology of the body, prolonged aberrant posture puts an increased strain on the musculoskeletal system that can result in a number of different pain presentations. Low back pain, sciatic-like pain down the legs, and pain in the hips are all common presentations in lower crossed syndrome. More specifically, a study performed by Rana et al, noted that superior cluneal nerve entrapment due to an increase in lumbar lordosis (curve) and an anterior pelvic tilt, both seen commonly in lower crossed syndrome, lead to increased muscle tightness which in turn entraps the superior cluneal nerve causing pain in the low back/hip area. This specific nerve and pain pattern is often overlooked when attempting to establish a root cause for an individual’s low back pain. Besides low back pain, prolonged muscle imbalance can lead to changes in the spine itself. Over time, lower crossed syndrome can lead to the increase in lumbar lordosis and a compensatory increase in thoracic kyphosis. This can increase the chances of spinal degeneration due to increased stress on the joints. Hypolordosis (flattening) of the lumbar spine can also occur during prolonged lower crossed syndrome, which can also lead to compensatory thoracic hyperkyphosis. Mid-back pain is one of the more common symptoms of having an increased thoracic kyphosis. Each person with lower crossed syndrome may present with similar or completely different symptoms. At the end of the day, it is the provider’s responsibility to be diligent and establish a course of care that is best suited to calm the effects of lower crossed syndrome.
How Chiropractic and Massage Therapy Can Help
At Lakeland Chiropractic, we take the time to evaluate each individual to determine a suitable course of care. Just because lower crossed syndrome is common does not mean treatment should be common. People respond differently to different kinds of care and there is no one size fits all model.
The first thing you can expect to happen here at Lakeland Chiropractic is a comprehensive exam to determine the root cause of your presenting symptoms. In the case of presenting with lower crossed syndrome commonalities, we will examine the low back, reflexes, sensory and motor function. Once deduced that the cause of your presenting symptoms are due to improper function of coordinating muscles and aberrant posture, chiropractic adjustment may be administered to aid in restoring proper joint mobility. From there we will look at the neurology of the muscles associated with lower crossed syndrome. Releasing the entrapped nerves from the hypertonic muscles will help ease the discomfort and ensure that the muscles have the opportunity to function properly in coordination with other muscles in the region. Progress will be monitored throughout the visits to the clinic and when symptoms subside to a more tolerable level, exercises can be demonstrated to help the patient manage their symptoms at home. We strive to provide effective and lasting treatment to all patients regardless of presenting conditions.
Massage therapy:
Massage therapy is a beneficial tool in combating the hypertonic muscles commonly seen with lower crossed syndrome. A variety of massage techniques can be beneficial to lengthening and relaxing the over active, hypertonic muscles. Along with helping the hypertonic muscles relax, massage can help stimulate the muscles that are weak/inhibited. This in turn can help the postural issues seen in lower crossed syndrome.
Closing:
You as a patient deserve to have the best care possible and here at Lakeland Chiropractic we strive to provide a unique approach that drives the best possible outcomes for the individual patient.
References
ERDEM, Hatice Rana, et al. “Superior Cluneal Nerve Entrapment Due to Lower Crossed Syndrome: A Case with Low Back Pain.” Agri Pain, vol. 34, no. 4, Oct. 2022, pp. 311–315., https://doi.org/10.147744/agri.2020.21703.
Fletcher, Jenna. “What to Know about Lower Cross Syndrome.” Edited by Angela M Bell, Medical News Today, 30 Oct. 2020, https://www.medicalnewstoday.com/articles/lower-cross-syndrome.
Gubbels. “Lower Cross Syndrome...A Primary Cause of Low Back Pain.” Squareonehealth.com/Lower-Cross-Syndrome-Part-1/, 19 Mar. 2021, https://www.physio-pedia.com/Lower_Crossed_Syndrome.
“Lower Cross Syndrome.” Crucial Rehab, 1 Dec. 2020, https://www.crucialrehab.com/post/lower-cross-syndrome. Accessed 7 Feb. 2023.
"Lower Crossed Syndrome." Physiopedia, .15 Dec 2022, 14:46 UTC. 2 Mar 2023, 17:14 <https://www.physio-pedia.com/index.php?title=Lower_Crossed_Syndrome&oldid=323323>.
Sabogal, Diego. “Lower Cross Syndrome Type A Posture.” Medical News Today, 30 Oct. 2020, https://www.medicalnewstoday.com/articles/lower-cross-syndrome#treatment. Accessed 7 Feb. 2023.
Sabogal, Diego. “Lower Cross Syndrome Type B Posture.” Medical News Today, 30 Oct. 2020, https://www.medicalnewstoday.com/articles/lower-cross-syndrome#treatment. Accessed 7 Feb. 2023.
Topic of the Month: Upper Crossed Syndrome
Upper Crossed Syndrome is an umbrella term to describe a group of related postural dysfunctions. There are several commonalities in persons who have this condition.
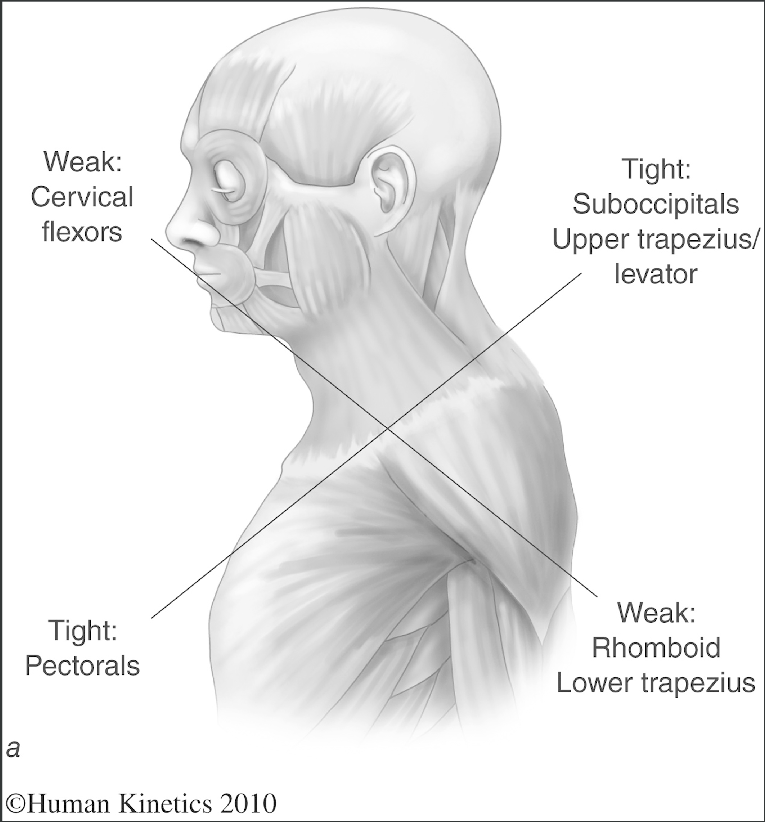
Upper Crossed Syndrome is an umbrella term to describe a group of related postural dysfunctions. There are several commonalities in persons who have this condition. They include but are not limited to a forward head position, shoulders that appear rounded forward, and a series of hypertonic (tight)/ weak muscles. The “crossed” term refers to the muscle patterns that are commonly seen in individuals. Hypertonic muscles that are commonly seen with this condition include pectoralis (pecs) muscles, upper trapezius muscles, suboccipital muscles, and levator scapula muscles. These hypertonic muscles tend to pull the shoulders forward and elevate them giving off a more rounded postural appearance. Weak muscle patterns develop in opposition to the hypertonic muscles. These muscles include cervical (neck) flexors, lower trapezius, and rhomboid muscles. The rhomboids are located between the shoulder blades and typically function to oppose the pectoralis muscles by pulling the shoulder blades together. Weakness of these muscles allow the pectoralis muscles to be more dominant, resulting in the appearance of rounded shoulders. Weakness in the lower trapezius muscles allows the upper trapezius and levator scapula muscles to essentially elevate the shoulders, compounding the forward rounding seen due to hypertonic pectoralis muscles. When cervical flexor muscles are weak/inhibited, head posture is affected by the appearance of a forward (anterior) head posture. These in turn create hypertonic suboccipital muscles due to the forward strain within the neck.
Combine these muscle patterns together and you get a cross-like presentation in muscle imbalance and notable postural changes.
Population Affected:
Upper crossed syndrome is becoming more and more prevalent in society today. With large portions of the population sitting behind desks and computers all day, the muscles listed above have an increased chance of developing into an upper crossed dysfunction. Poor sitting posture with head position straining forward toward the computer screen with hands outstretched to the keyboard puts the body in a disadvantageous position to combat upper crossed syndrome. Kids now commonly present with upper crossed syndrome due to excess time sitting on a computer or looking down at their phone for extended periods of time. The same can be said with an aging population; increased screen time, whether that be television, phone/tablet, or computer use can adversely affect everyone’s posture.
Effects of Upper Crossed Syndrome:
The effects of upper crossed syndrome vary from person to person. One of the most common effects is pain in the upper area of the back or between the shoulder blades. The hunched forward posture increases stress to that region of the body and can manifest in noticeable pain. Persons also may experience pain in the shoulders from this poor posture. Neck tension and pain is also commonly seen in upper crossed syndrome. This increase in tension and hypertonic suboccipital muscles in the posterior neck can lead to an increase in cervicogenic headaches. Cervicogenic headaches commonly present with pain near the base of the skull that can travel both up into a more traditional headache or progress down the neck leading to increased neck pain/aching. Tension headaches may also manifest from poor posture such as seen with upper crossed syndrome. This headache differs from cervicogenic headaches with a common presentation described as a band-like tension of pain around the head. In certain cases, pain, tingling and numbness could present in one or both arms. This can be due to compression of nerves and/or blood vessels from the shoulders being in the forward rounded position for extended periods of time.
How Chiropractic and Massage Therapy Can Help:
At Lakeland Chiropractic, we take the time to evaluate each individual to determine a suitable course of care. Just because upper crossed syndrome is common does not mean treatment should be common. People respond differently to different kinds of care and there is no one size fits all model.
Here at Lakeland Chiropractic We take a unique approach in determining the underlying cause of upper crossed syndrome. By looking into the neurology of upper crossed syndrome, we have found that nerve entrapment from the neck flowing down into the arms can lead to this chronic posture and associated symptoms. When nerves cannot properly function and become compressed they alter the biomechanics of our musculoskeletal system. By releasing the entrapped nerves, function can be restored in the associated muscles and joints. Patient’s often see dramatically decreased symptoms in a short period of time, when before they might have felt that they have tried everything and nothing seemed to last or help their issue at hand.
Chiropractic care can help relieve the tension in the upper back and neck with an adjustment to a specific vertebra which will help restore proper joint motion in the spine. Proper motion can help alleviate pain in the region that upper crossed syndrome can cause. Adjustments to the shoulder and clavicle can also help a person feel like they are more opened up in the chest and make it easier to retract the shoulder blades and feel less hunched over. The adjustment can also help with muscle relaxation for the hypertonic muscles.
Massage therapy is a beneficial tool in combating the hypertonic muscles commonly seen with upper crossed syndrome. A variety of massage techniques can be beneficial to lengthening and relaxing the over active, hypertonic muscles. Along with helping the hypertonic muscles relax, massage can help stimulate the muscles that are weak/inhibited.
While not specific to chiropractic or massage therapy, corrective exercises and stretching can be of huge benefit to the muscles and postural issues at hand.
Combining the two therapies with corrective exercises, you can get a more balanced and well functioning musculoskeletal system.